Laryngomalacia / Laryngomalazie, "floppy larynx"
(Kehlkopf und Luftröhre)
General information:
- Immaturity of the larynx, male preponderance, 60% of the laryngeal problems in infants.
- Shortened aryepiglottic folds, omega or tubular shaped epiglottis, anteriorly and medially-aligned collapsing movements of the arytenoid cartilages, excessive tissue in the supra - arytenoid area.
- Increasing inspiratory effort is followed by increasing obstruction.
Symptoms:
- Stridor (inspiratory fluttering noise; especially in the supine position), sometimes only during exercise (differential diagnosis: asthma, lack of fitness). Expiration is usually without a noise.
- Respiratory difficulties usually present within the first two weeks of life and symptoms may increase during the first months.
- Condition exacerbated by crying.
- Sometimes feeding problems.
- Symptoms usually resolve at the age of 2 with a benign clinical course.
Diagnostic workout:
- Physical examination.
- Respiratory function (blood gases, oxygen saturation monitoring, in severe cases ORCG is indicated).
- Direct flexible laryngo – bronchoscopy (child under topical or general anaesthesia, but breathing spontaneously, the scope passed through the nose and the epipharynx). In severe cases, the vocal cords cannot be seen because of the supraglottic collapse.
Indication for operation:
- Respiratory distress, phases of obstructive apnea and failure to thrive.
Treatment/Operation:
- Tracheostomy.
- Dissection (CO2 laser) of the shortened right and left aryepiglottic fold (picture).
- Possibly conservative unilateral or bilateral (typical) removal of supraglottic obstructive tissue: supraglottoplasty (caution: postoperative supraglottic stenosis from removal of too much tissue).
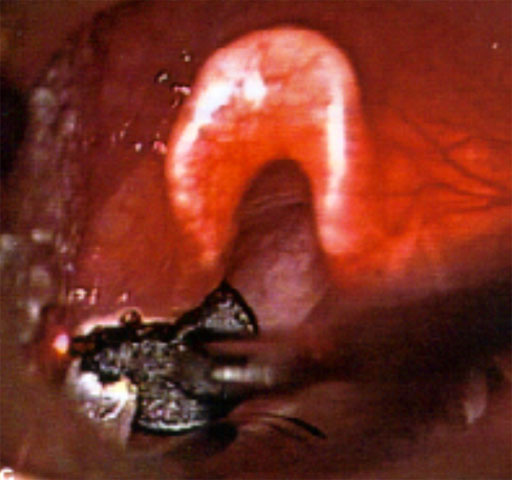
Laser dissection of the shortened left aryepiglottic fold (from Steiner W., Werner J.A.: Lasers in otorhinolaryngology. Head and neck surgery. Thieme 2000)
Postoperative management:
- Antibiotic management.
Prognosis:
- Usually good, self-limiting condition.
Laryngotracheal (subglottic) stenosis
(subglottische Stenose):
General information:
- Acquired or congenital.
- Usually after long term artificial ventilation in neonates by a tube related mucosa lesion (impaired blood perfusion due to a tight fitting tube – no air leak) in the area of the cricoid cartilage.
Symptoms:
- Stridor and respiratory distress.
- Recurrent croup like infections.
Diagnostic workout:
- Respiratory function (blood gases, oxygen saturation monitoring).
- Direct flexible laryngo – bronchoscopy (child spontaneously breathing; avoid intubation especially when high grade stenosis is suspected, risk of complete obstruction due to mucosa swelling. Prepare equipment for urgent tracheotomy). Anesthesia for laryngo - bronchoscopy: Propofol: 2 – 6 mg /kg IV. Fentanyl: 2 – 4
- Differential diagnosis: hemangioma, rarely lymphangioma. Describe the grade of stenosis (grade I: 0-50% obstruction, grade II:51-70% obstruction, grade III: 71-99% obstruction, grade IV: no detectable lumen). Endoscopy should be repeated every 6 months.
- In a full term infant a narrowing of the cricoid ring to less than 4mm in diameter and intubation with tube no. 3 is not possible (including the necessary air leak).
- Plain radiographs, CT or MRI scans are better, especially for measuring the length of the stenosis.
- Look for conjoined GER.
Indication for operation:
- Respiratory distress, phases of obstructive apnoea and failure to thrive.
- Stenosis grade III and more.
Treatment/Operation:
- Tracheotomy (time to grow, allow stenosis to mature, language skills delayed).
- During operative procedures jet – ventilation is superior.
- Laser incision/ablation in highly selected cases of low grade stenosis (4 quadrant incisions followed by dilatations). Problem: possible induction of scar tissue.
- Gentle dilatations in early stages including systemic steroids.
- Grade III and IV lesions require open reconstruction.
- Anterior cricoid split.
- Anterior and/or posterior cricoid split (extended 5 – 10 mm into the tracheal wall) with costal cartilage expansion (if required distraction is more than 3mm). Perichondrium should be preserved intact on the inner surface (for improved epithelialization) and removed on the outer surface.
Postoperative management:
- Repeated endoscopies at 4 weeks, 3 months, 6 months, 12 months and 24 months.
- Antibiotic management for 3 weeks to 1 month.
- Anti - GER treatment if necessary.
Prognosis:
- Endoscopy every 6 months.
Benign laryngeal tumors
(gutartige Kehlkopftumoren):
Papilloma (Papillom)
General information:
- The most common benign neoplasm of the larynx.
- Multiple locations (vocal cords and the anterior commissure), with possible extension into the distal airway.
- No histological differences between the juvenile and adult forms.
- Frequently detected between the ages of 2 and 5 years.
- Caused by the human papilloma virus (HPV-6, HPV-11).
- Discussion: 50% of children with recurrent respiratory papillomas have mothers with active cervical papillomas at birth.
Symptoms:
- Hoarseness.
- Respiratory insufficiency (extension into the distal airway).
Diagnostic workout:
- Respiratory function (blood gases, oxygen saturation monitoring).
- Direct flexible laryngo – bronchoscopy.
Indication for operation:
- Maintenance of the airway (20 - 30% require tracheotomy)
Treatment/Operation:
- Antiviral agents (alpha – interferon) with variable results.
- Laser ablation/vaporization (complications: scar tissue, fixation of the vocal cord).
- Tracheotomy.
Prognosis:
- Recurrence is typical over a certain period.
- There is no universally effective treatment.
Subglottic hemangioma (subglottisches Hämangiom)
General information:
- Rarely present at birth, develops within the first months of life.
- 50% also have cutaneous hemangiomas.
- Rapid growth generally subsides by the age of 1 (complete resolution by the age of 5).
- A compressible lesion, usually arising from the posterolateral aspect of the subglottis.
- Usually a history of complete resolution.
Symptoms:
- Stridor (in the early stages: inspiratory stridor).
- Respiratory distress.
Diagnostic workout:
- Respiratory function (blood gases, oxygen saturation monitoring).
- Direct flexible laryngo – bronchoscopy.
- Ultrasound to detect liver hemangiomas.
- Cardiac ultrasound.
Indication for operation:
- Maintenance of the airway.
Treatment/Operation:
- Steroid (dexamethason: 1 mg/kg/day) or alpha – interferon (330 to 1 million units/day) medication.
- Tracheotomy to bypass the lesion and to wait for regression.
- Intralesional laser vaporization (NdYAG laser) with postoperative intubation for about 1 week.
Prognosis:
- Involution.
Lymphangioma (Lymphangiom):
General information:
- 50% of the lymphangiomas are located in the head and neck area compressing the surrounding structures.
- Larynx involvement is rare.
- Three types: simplex (capillary), carvernous, cystic.
- 50% detected in the neonatal period.
Symptoms:
- Stridor, voice alteration.
- Respiratory distress.
Diagnostic workout:
- Respiratory function (blood gases, oxygen saturation monitoring).
- Direct flexible laryngo – bronchoscopy.
Indication for operation:
- Maintenance of the airway.
Treatment/Operation:
- Tracheotomy to bypass the lesion.
- Complete resection of the laryngeal lesions rarely possible.
- Draining of the cysts by partial resection.
- Injection of sclerosing agents (e.g. 33% glucose solution) into large cysts.
Prognosis:
- Multiple procedures required for success.
Tracheomalacia (Tracheomalazie):
General information:
- Intrinsic defect of the trachea. Inability of the cartilages to keep the trachea open during respiration.
- Unusually an obstruction (collapse) develops during expiration (due to positive intrathoracic pressure the flattened trachea collapses during expiration).
- In patients after corrected esophageal atresia type IIIb. The site of collapse is usually above the entry of the esophagotracheal fistula.
- Unusually severe symptoms when more than 20% of the lumen remains open during breathing cycles.
- Differential diagnoses: compression from outside, due to vascular malformations.
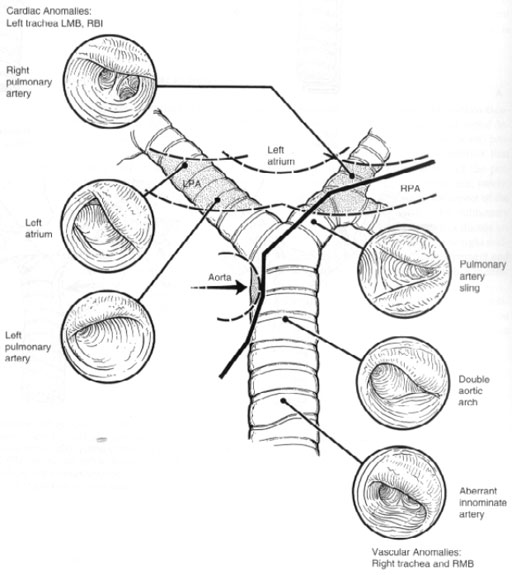
Vascular malformations leading to trachebronchial obstruction (from Holinger L.D. et al.: Pediatric Laryngology & Bronchoesophagology. Lippincott – Raven 1997)
Symptoms:
- Expiratory stridor.
- Respiratory distress.
Diagnostic workout:
- Respiratory function (blood gases, oxygen saturation monitoring).
- Direct flexible laryngo – bronchoscopy (child under local or general anaesthetic, but breathing spontaneously).
Indication for operation:
- Maintenance of the airway.
Treatment/Operation:
- Tracheotomy with an extra – long cannula to bypass the lesion.
- Aortopexy (left thoracotomy, resection of the left thymus lobe, suturing the aortic arch to the sternal periost with three CV3 Gore@ sutures taking several bites of the aortic adventitia, tie the sutures while the sternum is kept in a manually depressed position. When the sternum is released the anterior tracheal wall moves anteriorly).
- Division of the vascular ring.
- Endoluminal stents (problematic because of difficulties with removing and changing the device, problems with granulation tissue).
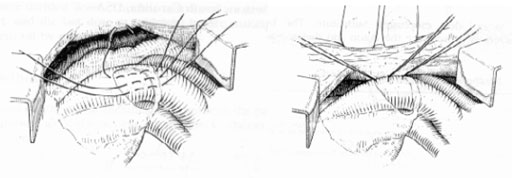
Aortopexy (from Spitz L., Coran A.: Pediatric Surgery. Chapman & Hall Medical 1995):
Prognosis:
- Good in cases treatable by simple aortopexy.



