Pleural effusion (Rippenfellergüsse, Pleuraergüsse)
Empyema:
General information:
- Bacterial infection of a pleural effusion following pneumonia (failure of medical therapy of parapneumonic effusions; 2/3 of the cases), thoracic surgery or trauma.
- Pneumococci and staphylococci remain the predominant organisms.
- Three stages of development (distinguished by radiographic, clinical and pleural fluid characteristics):
- Exudative phase: low WBC count, low LDH, normal glucose and pH levels.
- Fibrinopurulent phase: fibrin depositions producing a “peel” limiting the expansion of the lung, increasing WBC and LDH (> 1000 U/l) levels and a drop in glucose (< 40 mg/dL), increasing drainage difficulties.
- Organizing stage: thick fibrous inelastic “peel” with scar formation, lung entrapment, erosion of the lung or the chest wall (empyema necessitatis) is possible.
- A bronchopleural fistula may be involved (infected fluido – pneumothorax).
Symptoms:
- Fever, tachycardia, tachypnea, dyspnea, productive cough.
- Chest pain, reduced mobility of the chest wall at the affected site.
- Decreased breathing sounds and dullness to percussion on the involved side.
Diagnostic workout:
- Thoracic X-ray, CT scan or MRI (CT and MRI to differentiate between empyema and lung abscess).
- Additional determination of the empyema stage additionally by ultrasound (detection of the thick pleural peel).
- Needle thoracocentesis or (better) chest tube drainage. Aspirated fluid should be analyzed (Gram´s stain, aerobic and anaerobic cultures, search for mycobacteria, and fungi, WBC count, glucose level, LDH, pH). Sometimes ultrasound or CT assistance may be helpful for proper tube placement and successful thoracocentesis.
- Non-specific leukocytosis, drastically increased CRP levels.
Indication for operation:
- Late stage II (fibrinopurulent effusion).
- Effusion more than 3cm that does not improve after aggressive treatment (i.v. antibiotics, multiple drainage) over a period of 72h.
Treatment/Operation:
- In the early stages (exudative phase of parapneumonic empyema) administration of antimicrobial agents alone may be sufficient.
- Most empyemas require invasive interventions (large size chest tube drainage, thoracostomy or thoracotomy with decortication). It is better to drain than not to drain. Sometimes more than one chest tube is necessary to ensure adequate draining.
- If simple drainage fails intrapleural fibrinolytic agents (250.000 Units of Streptokinase or Urokinase in 100 ml of sterile saline; chest tubes remain clamped for at least for 4 hours) may be useful. Afterwards continuous suction on the chest tubes is necessary to increase the drained fluid volume and to expand the lung.
- Thoracoscopy is useful in the treatment of the multiloculated empyema when there is no thick visceral pleural peel. Simple debridement in the middle exudative phase is possible.
- Open drainage, lavage of the pleural cavity, via thoracotomy combined with decortication is indicated in the late fibrinopurulent and the organizig phase. The peel on the visceral pleura becomes a barrier to expansion, entrapping and immobilizing the lung. Decortication (major surgical procedure by removal of fibrin, polymorphonuclear white cells, macrophages and fibrous tissue, leaving the visceral pleura largely intact) allows reexpansion of the lung.
- In cases of bronchopleural fistula thoracotomy, open drainage and resection of the involved lung parenchyma is always necessary (usually a lobectomy). Bronchus closure may be reinforced by a dorsally based intercostal muscle flap.
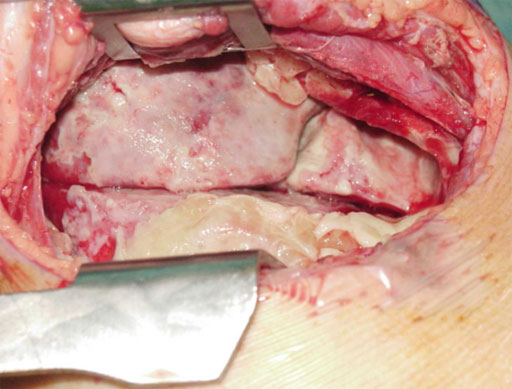
Early organization phase
Postoperative management:
- Chest tubes may be removed if the lung is fully expanded and drainage volumes fall below 20 to 50cc during a 24 hour period.
- Antibiotic management based on cultures should be continued until the chest tubes are removed and the pulmonary infection is controlled.
Prognosis:
- Lung entrapment from empyema is uncommon if the patient receives proper and timely (in terms of 3 phases) treatment.
Hemothorax:
General information:
- Blunt or penetrating trauma may produce a hemothorax (rib fractures). Frequently accompanied by a pneumothorax.
- Bleeding from the intercostal vessels, internal mammary vessels, or great vessels.
- Possible mediastinal shift.
Symptoms:
- Chest pain, decreased (no) breathing sounds and dullness to percussion on the involved side.
- Respiratory insufficiency.
- Depending on the blood loss (25% loss: prehypotensive, 40% loss: hypotensive - hypovolemic shock) increased heart rate, depressed levels of consciousness, decreased capillary refill, cold extremities, skin colour, decreased urinary output.
Diagnostic workout:
- Physical examination.
- Monitoring of the respiratory and circulatory status (blood gases, blood pressure, RBC count). Blood sample: RBC count, patients blood type.
- Venous access (peripheral, intraosseous, external and internal jugular vein, femoral vein, subclavian vein).
- Ultrasound, thoracic X-ray in an upright position (hemothorax may be missed in the supine position), volume substitution resuscitation should start simultaneously.
- Repeated thoracic X-ray (CT) to control drainage.
Treatment/Operation:
- Volume resuscitation is necessary: Initially 20 ml/kg BW of crystalloid improves the hemodynamic status (if necessary a second bolus). Eventually substitution of packed red blood cells (initial 10ml/kg BW). If type specific blood is not immediately available O – negative packed red blood cells can be given. Heart rate should drop, urine output should increase (1-2 ml/kg/h).
- Tube thoracostomy (early placement, large size for full drainage).
- Indications for operation are surgical hemostasis and complete drainage:
- Ongoing hemorrhage, if more than 20% of child’s blood volume is drained immediately (blood volume: 90ml/kg BW in a new-born, 80ml/kg BW at 1 year of age, 70ml/kg BW in early adolescence).
- Failure of complete drainage after several days. Via a limited thoracotomy evacuation of the clot and removal of pleural peel. Two chest drains should be placed.
Postoperative management:
- Chest tubes may be removed if the lung is fully expanded and drainage volumes fall below 20 to 50cc during a 24 hour period.
- Antibiotic management.
Prognosis:
- Persistent blood in the thorax increases the risk of empyema and lung entrapment.
Chylothorax:
General information:
- Accumulation of chyle in the pleural space.
- Physiologically the chyle from the right and left lumbar trunk flows into the left subclavian vein (angulus venosus) via the zysterna chyli and the thoracic duct (aortic hiatus, at the level of the 5th thoracic vertebrae inclining to the left).
- The thoracic duct has smooth muscles in the wall and valves.
- Common causes of pleural effusion in the first few days of life (malformations of the thoracic duct, birth trauma or unclear aetiology).
- Other causes: Insertion of a central venous line, postoperatively (cardiac surgery, operations in the mediastinum), chest tubes, blunt thoracic trauma, pneumonia, neoplasms).
- Chronic loss of T – cells (can lead to an impaired immunological status).
- Fluid and electrolyte imbalances, malnutrition.
- Possibly mediastinal shift.
Symptoms:
- Respiratory insufficiency (tachypnea), decreased (no) breathing sounds and dullness to percussion on the involved side.
- Lymphocytopenia as a consequence of chyle loss.
Diagnostic workout:
- Physical examination.
- Monitoring of the respiratory and circulatory status (blood gases, blood pressure, BC count).
- Ultrasound, thoracic X-ray in an upright position.
- Thoracocentesis (aspiration of a milky fluid after oral nutrition, chylomicrons, elevated numbers of lymphocytes).
Indication for operation:
- If chyle flow continues (more than 15ml/kg BW/day) for a period of 1 month (patient on TPN). This waiting reduces the need for surgical intervention!
Treatment/Operation:
- Repeated throracocentesis or chest tube to expand the lung.
- Total parenteral nutrition (no oral intake) to drastically decrease the chyle flow.
- Feedings restricted to medium – chain triglicerides (MCT).
- Operation:
- Try to detect the lesion by thoracoscopy or thoracotomy.
- Place surgical clips or multiple sutures, possibly ligation of the thoracic duct (main duct) above and below the leak.
- A pleuroperitoneal shunt may be effective.
- In resistant cases pleurodesis may be helpful.
Postoperative management:
- Chest tubes may be removed if the lung is fully expanded and drainage volumes fall below 20 to 50cc during a 24 hour period.
- No suction on the chest tubes.
- Antibiotic management.
Prognosis:
- Most chylothoraces resolve spontaneously.



